Abstract
Background: Cardiorenal syndrome (CRS) is a serious condition with high morbidity and mortality. Secondary CRS (type 5 CRS) is characterized by the coexistence of cardiac abnormality and renal dysfunction occurring secondarily to a systemic condition. In thalassemia, a common hematologic disease in Thailand, there is limited information about the prevalence of secondary CRS. Therefore, this study aimed to investigate the prevalence and associated risk factors of secondary CRS in thalassemia patients.
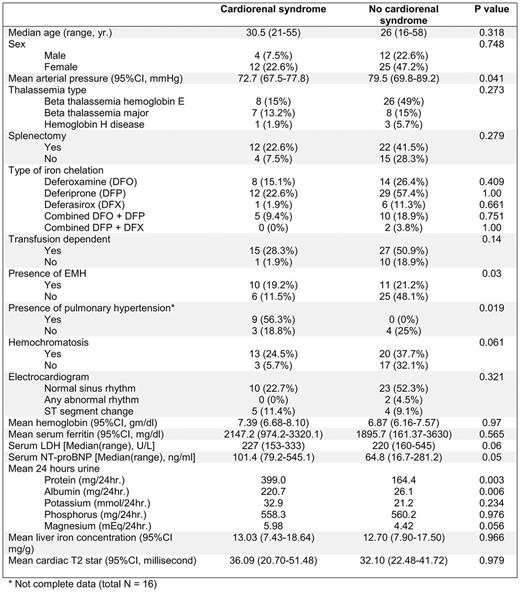
Method: In this cross-sectional cohort study, 53 adult thalassemia patients in out-patient clinic of Chiang Mai University Hospital since October 2016 to June 2017 were included. A criterion for diagnosis of secondary CRS is based on a system proposed by Ronco and McCullough. Cardiac abnormalities, assessed by clinical presentation of heart failure, chest X-ray, electrocardiogram, and echocardiogram, included acute or chronic heart failure by using definition from 2016 ESC guideline or structural cardiac abnormalities defined by LV remodeling and dysfunction, diastolic dysfunction, chronic abnormalities in cardiac function or cardiomyopathy. Renal dysfunction is defined by acute kidney injury or chronic kidney according to 2012 KDIGO guidelines. Clinical and laboratory (serum NT-proBNP, spot urine protein, spot urine albumin, spot urine electrolytes, 24-hours urine protein, and 24-hour urine electrolytes) data for 2 consecutive visits, at least three months apart, were assessed. We analyzed correlation between patients with and without cardiorenal syndrome by Chi-square for categorical data, T-test and non-parametric test of 2 independent samples for continuous data. We used binary logistic regression model for multivariate analysis.
Result: Of 53 thalassemia patients [42 (79.2%) transfusion dependent thalassemia and 11 (20.8%) non-transfusion dependent thalassemia], 16 (30.2%) has secondary CRS. Cardiac abnormalities was detected in 23 patients (43.4%), included acute or chronic heart failure (N=4, 7.5%), or structural cardiac abnormalities (N=23, 43.4%). Thirty-one patients (58.5%) had renal abnormalities. Compared with the non-CRS group, the CRS group had a significant increase in serum NT-proBNP level [median (range) = 101.4 (79.2-545.1) VS. 64.8 (16.7-281.2) ng/ml, p=0.05], 24-hours urine magnesium level [mean (95%CI) = 5.98 (3.91-8.04) VS. 4.42 (3.01-5.83) mEq/24 hr., p=0.042], 24-hours urine protein level [median (range) = 249 (132-1610) VS. 161 (77-324) mg/24 hr., p=0.003], and 24-hours urine albumin level [median (range) = 45 (3-1303) VS. 5 (2-184) mg/24 hr., p=0.006], but significance lower in mean arterial pressure (MAP) [mean (95%CI) = 72.7(67.5-77.8) VS. 79.5(69.8-89.2) mmHg, p=0.041]. In univariate analysis, CRS was associated with pulmonary hypertension (OR 2.33, p=0.019), presence of extramedullary hematopoiesis (EMH) (OR 3.79, p=0.03). Multivariate analysis confirmed the association of cardiorenal syndrome with presence of EMH (OR 6.55, p=0.04), lower MAP (OR 0.869, p=0.012), elevated serum NT-proBNP (OR =1.013, p=0.012), and elevated 24-hour urine magnesium (OR 2.17, p=0.004). There was no correlation of CRS with type of thalassemia, serum ferritin, liver iron concentration, cardiac T2* and type of iron chelating agents.
Conclusion: This study has demonstrated that CRS is common in thalassemia patients. Patients with the presence of EMH, low MAP, increased 24-hour urine magnesium level or an elevated serum NT-proBNP level are at high risk for developing CRS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal